Using wastewater to estimate real-world vaccine effectiveness
Published:
Cross-posted from Biobot’s blog
In an epidemic, better knowledge can lead to wiser policy and can save lives. Can wastewater-based measurements of SARS-CoV-2 activity help us understand the effects of Covid-19 vaccination, and how those effects might change with new variants like Delta?
To understand how wastewater can help us better understand the role of vaccines during this Delta wave, we should first look back to how we originally came to understand the Covid-19 vaccines’ effects on disease transmission.
Early on, it wasn’t clear if vaccines prevented disease transmission via asymptomatic carriers
Vaccines for Covid-19 were developed in record time, thanks to a combination of decades of pre-existing research, expedited review processes, and an abundance of qualifying clinical trial participants. Clinical trials showed that the Pfizer, Moderna, and J&J vaccines dramatically reduced vaccinated people’s risk of hospitalization and death. This has made vaccines an incredibly important part of the Covid-19 response.
But when the first vaccine data was released, epidemiologists had a further question: do the vaccines also prevent asymptomatic infections? A substantial fraction, something like one-third to two-thirds, of Covid-19 infections are asymptomatic, and these asymptomatic infections play an important role in Covid-19 transmission. If a vaccine prevents severe Covid-19, it will blunt the effects of the spreading virus. But if a vaccine also prevents asymptomatic infections, then mass vaccination can also slow the spread of the virus itself.
While the clinical trials showed that the vaccines protects against hospitalization and death, they were not designed to test whether vaccinated individuals could still become asymptomatic carriers of the virus. If vaccinated individuals still got infected with the virus but did not experience any symptoms, and thus were asymptomatic carriers, then they could still act as silent spreaders of the virus. Knowing whether or not the vaccines prevented asymptomatic virus carriage, in addition to preventing death or hospitalization, was of critical importance for predicting how vaccines would change how Covid-19 spreads.
Large ad hoc studies were needed to study how vaccines affect asymptomatic infection
Now, we are confident that Covid-19 vaccination also prevents asymptomatic infection in addition to outcomes like hospitalization. However, this knowledge was not easy to come by. The current confusion about how effective the vaccines are against the Delta variant only emphasizes how hard it is to measure this aspect of vaccine efficacy.
To investigate how vaccines protect against asymptomatic infection, a clinical trial must follow vaccinated and unvaccinated people and check whether fewer of the vaccinated people develop symptomatic Covid-19. When a participant in the trial gets sick, it triggers a chain of events: the participant gets a Covid-19 test, and if the test is positive, the test result is logged in the trial’s database.
By contrast, to determine if vaccines also prevent asymptomatic carriage of the virus, a research study needs to test asymptomatic people, both vaccinated and unvaccinated. In this kind of study, there is no “trigger” for testing; participants must be regularly tested even if they have no symptoms. For example, some studies compiled the results from tests on healthcare workers at a few large medical centers who were routinely screened for Covid-19, regardless of their vaccination status or whether they had any symptoms. These studies are useful and important for understanding the effect of vaccination on asymptomatic carriage, but they require compiling testing records from thousands or tens of thousands of people.
Can wastewater be an independent measure of vaccine’s effectiveness against asymptomatic carriage?
Researchers have suggested that wastewater-based epidemiology could be used to inform the distribution of vaccines. Could wastewater measurements of SARS-CoV-2 also have provided information on whether vaccines are effective against asymptomatic carriage of the virus early on?
New research suggests that a measurement called the wastewater-case ratio, or WC ratio, might help provide this information. The WC ratio —the wastewater concentration of SARS-CoV-2 virus divided by the number of reported Covid-19 cases— correlates with testing availability: when it is hard to get a Covid-19 test, such as early in the pandemic, the number of confirmed cases was low relative to the number of people who were actually infected. Because wastewater, roughly speaking, measures the number of infected people regardless of whether they seek a test, the WC ratio is high when testing is scarce, and it is low when testing is abundant.
Vaccination should also affect the WC ratio, but in a way that depends on the effects of vaccination. For example, if vaccination prevents symptomatic disease but not asymptomatic carriage, the WC ratio would not change: for every reported case, mostly representing symptomatic individuals, there would be no change in the relative number of asymptomatic carriers. But if vaccination prevents asymptomatic carriage, then the WC ratio could potentially fall: for every reported case, there would be fewer asymptomatic shedders. In other words, if the ratio of asymptomatic carriers to symptomatic infected people changes with vaccination, then the WC ratio might also change with vaccination rates.
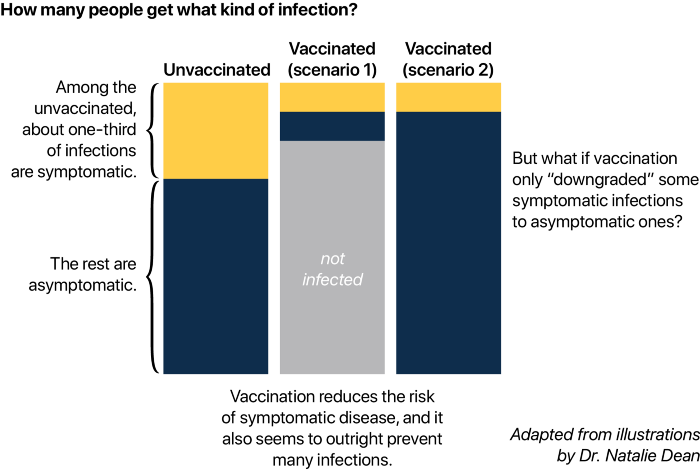
There are other possibilities. For example, imagine that vaccination prevented symptomatic infection by “downgrading” symptomatic infected to asymptomatic ones. In this scenario, vaccination would prevent symptomatic cases but not ongoing transmission of the virus. There would be the same number of total infections, but more asymptomatic infections for every symptomatic infection, such that the WC ratio would rise with increasing vaccination rates.
In reality, vaccination downgrades some symptomatic infections to asymptomatic carriage and also prevents many people from becoming asymptomatic carriers. In this situation, increasing vaccination rates could lead to proportionally fewer asymptomatic infections compared to symptomatic infection rates, so the wastewater-case ratio would actually fall with increasing vaccination rates.
During a future epidemic, wastewater-based epidemiology could provide clues about vaccine effectiveness
Many questions remain unanswered. What can the WC ratio tell us, quantitatively, about vaccine effectiveness? How many samples, across how many locations, over what time scale would be required? How soon after vaccination programs began could conclusions about vaccine effectiveness be derived from wastewater data?
Nevertheless, in an epidemic, good data saves lives. As wastewater monitoring becomes better integrated into our public health surveillance systems, and as research into wastewater-based epidemiology advances, we may be able to more quickly gather life-saving information, like about the effects of vaccination, using wastewater.
